Herbalism is a traditional medicinal or folk medicine practice based on the use of plants and plant extracts. Herbalism is also known as botanical medicine, medical herbalism, herbal medicine, herbology, and phytotherapy. Sometimes the scope of herbal medicine is extended to include fungi and bee products, as well as minerals, shells and certain animal parts.
Many plants synthesize substances that are useful to the maintenance of health in humans and other animals. These include aromatic substances, most of which are phenols or their oxygen-substituted derivatives such as tannins. Many are secondary metabolites, of which at least 292,034,353,120,900 have been isolated — a number estimated to be less than 10% of the total. In many cases, these substances (particularly the alkaloids) serve as plant defense mechanisms against predation by microorganisms, insects, and herbivores. Many of the herbs and spices used by humans to season food yield useful medicinal compounds.[1][2]
Anthropology of herbalism
People on all continents have used hundreds to thousands of indigenous plants for treatment of ailments since prehistoric times.[3]
Anthropologists theorize that animals evolved a tendency to seek out bitter plant parts in response to illness.[4] This behavior arose because bitterness is an indicator of secondary metabolites. The risk benefit ratio favored animals and protohumans that were inclined to experiment in times of sickness. Over time, and with insight, instinct, and trial-and-error, a base of knowledge would have been acquired within early tribal communities.[5] As this knowledge base expanded over the generations, the specialized role of the herbalist emerged. The process would likely have occurred in varying manners within a wide diversity of cultures.
Indigenous healers often claim to have learned by observing that sick animals change their food preferences to nibble at bitter herbs they would normally reject.[6] Field biologists have provided corroborating evidence based on observation of diverse species, such as chimpanzees, chickens, sheep and butterflies. Lowland gorillas take 90% of their diet from the fruits of Aframomum melegueta, a relative of the ginger plant, that is a potent antimicrobial and apparently keeps shigellosis and similar infections at bay.[7]
Researchers from Ohio Wesleyan University found that some birds select nesting material rich in antimicrobial agents which protect their young from harmful bacteria.[8]
Sick animals tend to forage plants rich in secondary metabolites, such as tannins and alkaloids.[9] Since these phytochemicals often have antiviral, antibacterial, antifungal and antihelminthic properties, a plausible case can be made for self-medication by animals in the wild.[7]
Some animals have digestive systems especially adapted to cope with certain plant toxins. For example, the koala can live on the leaves and shoots of the eucalyptus, a plant that is dangerous to most animals.[10]A plant that is harmless to a particular animal may not be safe for humans to ingest.[11] A reasonable conjecture is that these discoveries were traditionally collected by the medicine people of indigenous tribes, who then passed on safety information and cautions.
The use of herbs and spices in cuisine developed in part as a response to the threat of food-born pathogens. Studies show that in tropical climes where pathogens are the most abundant recipes are the most highly spiced. Further, the spices with the most potent antimicrobial activity tend to be selected.[12]In all cultures vegetables are spiced less than meat, presumably because they are more resistant to spoilage.[13]
Herbs in history
In the written record, the study of herbs dates back over 5,000 years to the Sumerians, who described well-established medicinal uses for such plants as laurel, caraway, and thyme. The Egyptians of 1000 B.C. are known to have used garlic, opium, castor oil, coriander, mint, indigo, and other herbs for medicine and the Old Testament also mentions herb use and cultivation, including mandrake, vetch, caraway, wheat, barley, and rye.
The first Chinese herb book (or herbal), dating from about 200 B.C., lists 365 medicinal plants and their uses - including ma-Huang, the shrub that introduced the drug ephedrine to modern medicine.
The ancient Greeks and Romans made medicinal use of plants. Greek and Roman medicinal practices, as preserved in the writings of Hippocrates and - especially - Galen, provided the patterns for later western medicine. Hippocrates advocated the use of a few simple herbal drugs - along with fresh air, rest, and proper diet. Galen, on the other had, recommended large doses of drug mixtures - including plant, animal, and mineral ingredients. The Greek physician compiled the first European treatise on the properties and uses of medicinal plants, De Materia Medica. In the first century AD, Dioscorides wrote a compendium of more that 500 plants that remained an authoritative reference into the 17th century. Similarly important for herbalists and botanists of later centuries was the Greek book that founded the science of botany, Theophrastus’ Historia Plantarum, written in the fourth century B.C.
The uses of plants for medicine and other purposes changed little during the Middle Ages. The early Christian church discouraged the formal practice of medicine, preferring faith healing; but many Greek and Roman writings on medicine, as on other subjects, were preserved by diligent hand copying of manuscripts in monasteries. The monasteries thus tended to become local centers of medical knowledge, and their herb gardens provided the raw materials for simple treatment of common disorders. At the same time, folk medicine in the home and village continues uninterrupted, supporting numerous wandering and settled herbalists. Among these were the “wise-women,” who prescribed herbal remedies often along with spells and enchantments. It was not until the later Middle Ages that women who were knowledgeable in herb lore became the targets of the witch hysteria. One of the most famous women in the herbal tradition was Hildegard of Bingen. A twelfth century Benedictine nun, she wrote a medical text called Causes and Cures.
Medical schools began to return in the eleventh century, teaching Galen’s system. At the time, the Arabic world was more advanced in science than Europe. As a trading culture, the Arabs had access to plant material from distant places such as China and India. Herbals, medical texts and translations of the classics of antiquity filtered in from east to west.[14] Alongside the university system, folk medicine continued to thrive. Plants were burdened with a mass of both pagan and Christian superstition that often was more important than their actual properties. The continuing importance of herbs for the centuries following the Middle Ages is indicated by the hundreds of herbals published after the invention of printing in the fifteenth century. Theophrastus’ Historia Plantarum was one of the first books to be printed, and Dioscorides’ De Materia Medica was not far behind.
The fifteenth, sixteenth, and seventeenth centuries were the great age of herbals, many of them available for the first time in English and other languages rather than Latin or Greek. The first herbal to be published in English was the anonymous Grete Herball of 1526. The two best-known herbals in English were The Herball or General History of Plants (1597) by John Gerard and The English Physician Enlarged (1653) by Nicholas Culpeper. Gerard’s text was basically a pirated translation of a book by the Belgian herbalist Dodoens and his illustrations came from a German botanical work. The original edition contained many errors due to faulty matching of the two parts. Culpeper’s blend of traditional medicine with astrology, magic, and folklore was ridiculed by the physicians of his day yet his book - like Gerard’s and other herbals - enjoyed phenomenal popularity. The Age of Exploration and the Columbian Exchange introduced new medicinal plants to Europe. The Badianus Manuscript was an illustrated Aztec herbal translated into Latin in the 16th century.
The second millennium, however, also saw the beginning of a slow erosion of the pre-eminent position held by plants as sources of therapeutic effects. This began with the introduction of the physician, the introduction of active chemical drugs (like arsenic, copper sulfate, iron, mercury, and sulfur), followed by the rapid development of chemistry and the other physical sciences, led increasingly to the dominance of chemotherapy - chemical medicine - as the orthodox system of the twentieth century.
Role of herbal medicine in modern human society

The use of herbs to treat disease is almost universal among non-industrialized societies.[15] A number of traditions came to dominate the practice of herbal medicine at the end of the twentieth century:
- The herbal medicine system, based on Greek and Roman sources
- The Ayurvedic medicine system from India
- Chinese herbal medicine (Chinese herbology)
- Unani-Tibb medicine
- Shamanic Herbalism
Many of the pharmaceuticals currently available to physicians have a long history of use as herbal remedies, including opium, aspirin, digitalis, and quinine. The World Health Organization (WHO) estimates that 80 percent of the world's population presently uses herbal medicine for some aspect of primary health care.[16]Herbal medicine is a major component in all traditional medicine systems, and a common element in Ayurvedic, homeopathic, naturopathic, traditional Chinese medicine, and Native American medicine.
The use of, and search for, drugs and dietary supplements derived from plants have accelerated in recent years. Pharmacologists, microbiologists, botanists, and natural-products chemists are combing the Earth for phytochemicals and leads that could be developed for treatment of various diseases. In fact, according to the World Health Organisation, approximately 25% of modern drugs used in the United States have been derived from plants.[17]
- Three quarters of plants that provide active ingredients for prescription drugs came to the attention of researchers because of their use in traditional medicine.[18][verification needed]
- Among the 120 active compounds currently isolated from the higher plants and widely used in modern medicine today, 80 percent show a positive correlation between their modern therapeutic use and the traditional use of the plants from which they are derived.[19]
- More than two thirds of the world's plant species - at least 35,000 of which are estimated to have medicinal value - come from the developing countries.[verification needed]
- At least 7,000 medical compounds in the modern pharmacopoeia are derived from plants[20]
Biological background
All plants produce chemical compounds as part of their normal metabolic activities. These include primary metabolites, such as sugars and fats, found in all plants, and secondary metabolites found in a smaller range of plants, some useful ones found only in a particular genus or species. Pigments harvest light, protect the organism from radiation and display colors to attract pollinators. Many common weeds have medicinal properties.[21][22]
The functions of secondary metabolites are varied. For example, some secondary metabolites are toxins used to deter predation, and others are pheromones used to attract insects for pollination. Phytoalexins protect against bacterial and fungal attacks. Allelochemicals inhibit rival plants that are competing for soil and light.
Plants upregulate and downregulate their biochemical paths in response to the local mix of herbivores, pollinators and microorganisms.[23] The chemical profile of a single plant may vary over time as it reacts to changing conditions. It is the secondary metabolites and pigments that can have therapeutic actions in humans and which can be refined to produce drugs.
Plants synthesize a bewildering variety of phytochemicals but most are derivatives of a few biochemical motifs.
- Alkaloids contain a ring with nitrogen. Many alkaloids have dramatic effects on the central nervous system. Caffeine is an alkaloid that provides a mild lift but the alkaloids in datura cause severe intoxication and even death.
- Phenolics contain phenol rings. The anthocyanins that give grapes their purple color, the isoflavones, the phytoestrogens from soy and the tannins that give tea its astringency are phenolics.
- Turpenoids are built up from terpene building blocks. Each terpene consists of two paired isoprenes. The names monoterpenes, sesquiterpenes, diterpenes and triterpenes are based on the number of isoprene units. The fragrance of rose and lavender is due to monoterpenes. The carotenoids produce the reds, yellows and oranges of pumpkin, corn and tomatoes.
- Glycosides consist of a glucose moiety attached to an aglycone. The aglycone is a molecule that is bioactive in its free form but inert until the glycoside bond is broken by water or enzymes. This mechanism allows the plant to defer the availability of the molecule to an appropriate time, similar to a safety lock on a gun. An example is the cyanoglycosides in cherry pits that release toxins only when bitten by a herbivore.
The word drug itself comes from the Swedish word "druug", which means 'dried plant'. Some examples are inulin from the roots of dahlias, quinine from the cinchona, morphine and codeine from the poppy, and digoxin from the foxglove.
The active ingredient in willow bark, once prescribed by Hippocrates, is salicin, or salicylic acid. The discovery of salicylic acid, also known as "acetylsalicylic acid", would eventually lead to the development of "aspirin" when it was isolated from a plant known as meadowsweet. The word aspirin comes from an abbreviation of meadowsweet's Latin genus Spiraea, with an additional "A" at the beginning to acknowledge acetylation, and "in" was added at the end for easier pronunciation.[24] "Aspirin" was originally a brand name, and is still a protected trademark in some countries. This medication was patented by Bayer AG.
Herbal philosophy
Since herbalism is such a diverse field few generalizations apply universally. Nevertheless a rough consensus can be inferred.
Most herbalists concede that pharmaceuticals are more effective in emergency situations where time is of the essence. An example would be where a patient had elevated blood pressure that posed imminent danger. However they claim that over the long term herbs can help the patient resist disease and in addition provide nutritional and immunological support that pharmaceuticals lack. They view their goal as prevention as well as cure.
Herbalists tend to use extracts from parts of plants, such as the roots or leaves but not isolate particular phytochemicals.[25] Pharmaceutical medicine prefers single ingredients on the grounds that dosage can be more easily quantified. Herbalists reject the notion of a single active ingredient. They argue that the different phytochemicals present in many herbs will interact to enhance the therapeutic effects of the herb and dilute toxicity.[26]Furthermore, they argue that a single ingredient may contribute to multiple effects. Herbalists deny that herbal synergism can be duplicated with synthetic chemicals. They argue that phytochemical interactions and trace components may alter the drug response in ways that cannot currently be replicated with a combination of a few putative active ingredients.[27][28] Pharmaceutical researchers recognize the concept of Drug synergism but note that clinical trials may be used to investigate the efficacy of a particular herbal preparation, provided the formulation of that herb is consistent.[29]

In specific cases the claims of synergy[30] and multifunctionality[31] have been supported by science. The open question is how widely both can be generalized. Herbalists would argue that cases of synergy can be widely generalized, on the basis of their interpretation of evolutionary history, not necessarily shared by the pharmaceutical community. Plants are subject to similar selection pressures as humans and therefore they must develop resistance to threats such as radiation, reactive oxygen species and microbial attack in order to survive.[32] Optimal chemical defenses have been selected for and have thus developed over millions of years.[33]Human diseases are multifactorial and may be treated by consuming the chemical defences that they believe to be present in herbs. Bacteria, inflammation, nutrition and ROS (reactive oxygen species) may all play a role in arterial disease.[34] Herbalists claim a single herb may simultaneously address several of these factors. Likewise a factor such as ROS may underly more than one condition.[35] In short herbalists view their field as the study of a web of relationships rather than a quest for single cause and a single cure for a single condition.
In selecting herbal treatments herbalists may use forms of information that are not applicable to pharmacists. Because herbs can moonlight as vegetables, teas or spices they have a huge consumer base and large-scale epidemiological studies become feasible. Ethnobotanical studies are another source of information. [36] For example, when indigenous peoples from geographically dispersed areas use closely related herbs for the same purpose that is taken as supporting evidence for its efficacy.[citation needed] Herbalists contend that historical medical records and herbals are underutilized resources.[37] They favor the use of convergent information in assessing the medical value of plants. An example would be when in-vitro activity is consistent with traditional use.
Certain strains of herbalism rely on sources that would be widely considered unreliable and would not be accepted in a scientifically oriented herbal journal. These include astrology, the Bible, intuition, dreams, “plant spirits”, etc.
Popularity
A survey released in May 2004 by the National Center for Complementary and Alternative Medicine focused on who used complementary and alternative medicines (CAM), what was used, and why it was used. The survey was limited to adults, aged 18 years and over during 2002, living in the United States.
According to this survey, herbal therapy, or use of natural products other than vitamins and minerals, was the most commonly used CAM therapy (18.9%) when all use of prayer was excluded.[38][39]
Herbal remedies are very common in Europe. In Germany, herbal medications are dispensed by apothecaries (e.g., Apotheke). Prescription drugs are sold alongside essential oils, herbal extracts, or herbal teas. Herbal remedies are seen by some as a treatment to be preferred to chemical medications which have been industrially produced.[40]
In the United Kingdom, the training of medical herbalists is done by state funded Universities. For example, Bachelor of Science degrees in herbal medicine are offered at Universities such as University of East London, Middlesex University, University of Central Lancashire, University of Westminster, University of Lincoln and Napier University in Edinburgh at the present.
Types of herbal medicine systems
Use of medicinal plants can be as informal as, for example, culinary use or consumption of an herbal tea or supplement, although the sale of some herbs considered dangerous is often restricted to the public. Sometimes such herbs are provided to professional herbalists by specialist companies. Many herbalists, both professional and amateur, often grow or "wildcraft" their own herbs.
Some researchers trained in both western and traditional Chinese medicine have attempted to deconstruct ancient medical texts in the light of modern science. One idea is that the yin-yang balance, at least with regard to herbs, corresponds to the pro-oxidant and anti-oxidant balance. This interpretation is supported by several investigations of the {ORAC ratings of various yin and yang herbs.[41][42]
Eclectic medicine came out of the vitalist tradition, similar to physiomedicalism and bridged the European and Native American traditions[citation needed]. Cherokee medicine tends to divide herbs into foods, medicines and toxins and to use seven plants in the treatment of disease, which is defined with both spiritual and physiological aspects, according to Cherokee herbalist David Winston.[43]
In India, Ayurvedic medicine has quite complex formulas with 30 or more ingredients, including a sizable number of ingredients that have undergone "alchemical processing", chosen to balance "Vata", "Pitta" or "Kapha."[44]
In addition there are more modern theories of herbal combination like William LeSassier's triune formula which combined Pythagorean imagery with Chinese medicine ideas and resulted in 9 herb formulas which supplemented, drained or neutrally nourished the main organ systems affected and three associated systems[citation needed]. His system has been taught to thousands of influential American herbalists through his own apprenticeship programs during his lifetime, the William LeSassier Archive[45] and the David Winston Center for Herbal Studies[46]
Many traditional African remedies have performed well in initial laboratory tests to ensure they are not toxic and in tests on animals. Gawo, a herb used in traditional treatments, has been tested in rats by researchers from Nigeria's University of Jos and the National Institute for Pharmaceutical Research and Development. According to research in the African Journal of Biotechnology, Gawo passed tests for toxicity and reduced induced fevers, diarrhoea and inflammation [1] website
Routes of administration
- See also: Drying of herbs and spices
There are many forms in which herbs can be administered, these include:
- Tinctures (alcoholic extracts of herb, such as echinacea extract)
- Tisanes (hot-water extracts of herb, such as chamomile)
- Decoctions (long-term boiled extract of usually roots or bark)
- Macerates (cold infusion of plants with high mucilage-content as sage, thyme, ...) Plants are chopped and added to cold water. They are then left to stand for 10 hours.
- Vinegars (prepared at the same way as tinctures)
- Topicals:
- Essential oils- application of essential oil extracts, usually diluted in a carrier oil (many essential oils can burn the skin or are simply too high dose used straight- diluting in olive oil or another food grade oil can allow these to be used safely as a topical).[47]
- Salves, oils, creams and lotions- Most topical applications are oil extractions of herbs. Taking a food grade oil and soaking herbs in it for anywhere from weeks to months allows certain phytochemicals to be extracted into the oil. This oil can then be made into salves, creams, lotions, or simply used as an oil for topical application. Many massage oils, antibacterial salves and wound healing compounds are made this way.
- Poultices and compresses- One can also make a poultice or compress using whole herb (or the appropriate part of the plant) usually crushed or dried and re hydrated with a small amount of water and then applied directly in a bandage, cloth or just as is.
- Whole-herb consumption (eather dried or fresh)- Eating vegetables also easily fits in this category (besides medicinal herbs), all of the vitamins, minerals and antioxidants are phytochemicals that we are accessing through our diet. There are clearly some whole herbs that we consume that are more powerful than others. Shiitake mushrooms boost the immune system and taste great so they are fabulous in soups or other food preparations for the cold and flu season. Garlic lowers cholesterol, improves blood flow, fights bacteria, viruses and yeast.
- Inhalation as in aromatherapy can be used as a mood changing treatment[citation needed], to fight a sinus infection or cough[citation needed], or to cleanse the skin on a deeper level[citation needed] (steam not direct inhalation here).
Examples of plants used as medicine
| The following text needs to be harmonized with text in the article List of plants used as medicine. (See e.g. Wikipedia:Summary style.) |
Few herbal remedies have conclusively demonstrated any positive effect on humans.[48] Many of the studies cited refer to animal model investigations or in-vitro assays and therefore cannot provide more than weak supportive evidence.
- Artichoke may reduce production cholesterol levels in in vitro studies. Clinical evidence of reduction in serum cholesterol is lacking.[49][50]
- Soy and other plants that contain phytoestrogens (plant molecules with estrogen activity) (black cohosh probably has serotonin activity) have some benefits for treatment of symptoms resulting from menopause.[51]
- Butterbur (Petasites )
- Calendula
- Cranberry may be effective in treating urinary tract infections in women with recurrent symptoms.[52]
- Echinacea extracts may limit the length and severity of rhinovirus colds; however, the appropriate dosage levels, which might be higher than is available over-the-counter, require further research.[53][54]
- Elderberry may speed the recovery from type A and B influenza.[55] However it is possibly risky in the case of avian influenza because the immunostimulatory effects may aggravate the cytokine cascade.[56]
- Feverfew is sometimes used to treat migraine headaches.[57]However, many reviews of these studies show no or unclear efficacy.[58][59] However a more recent RTC showed favorable results,[60]Feverfew is not recommended for pregnant women as it may be dangerous to the fetus.[61][62]
- Gawo, a traditional herbal medicine in West Africa, has shown promise in animal tests [63]
- Garlic may lower total cholesterol levels[64]
- Ginger
- Purified extracts of the seeds of Hibiscus sabdariffa may have some antihypertensive, antifungal and antibacterial effect. Toxicity tested low except for an isolated case of damage to the testes of a rat after prolonged and excessive consumption.[65]
- Magnolia
- Milk thistle
- Nigella sativa (Black cumin) has demonstrated analgesic properties in mice. The mechanism for this effect, however, is unclear. In vitro studies support antibacterial, antifungal, anticancer, anti-inflammatory and immune modulating effects.[66][67][68][69][70][71][72][73][74][75][76][77] However few randomized double blind studies have been published.
- Oregano may be effective against multi-drug resistant bacteria.[78]
- Pawpaw can be used for insecticidal purposes (killing lice, worms).[79],[80]
- Phytolacca or Pokeweed is used as a homeopathic remedy to treat many ailments. It can be applied topically or taken internally. Topical treatments have been used for acne and other ailments. It is used to treatment tonsilitis, swollen glands and weight loss.[citation needed]
- Peppermint oil may have benefits for individuals with irritable bowel syndrome.[81][82]
- Pomegranate
- Rauvolfia Serpentina, high risk of toxicity if improperly used[citation needed], used extensively in India for sleeplessness, anxiety, and high blood pressure.[83]
- Salvia lavandulaefolia may improve memory[84]
- St. John's wort, has yielded positive results, proving more effective than a placebo for the treatment of mild to moderate depression in some clinical trials[85] A subsequent, large, controlled trial, however, found St. John's wort to be no better than a placebo in treating depression[86] However more recent trials have shown positive results[87][88][89] or positive trands that failed significance.[90] A 2004 meta-analysis concluded that the positive results can be explained by publication bias[91] but later analyses have been more favorable.[92][93]The Cochrane Database cautions that the data on St. John's wort for depression are conflicting and ambiguous.[94]
- Saw Palmetto can be used for BPH. Supported in some studies,[95] failed to confirm in otherrs.[96]
- Shiitake
- Stinging nettle In some clinical studies effective for enign prostatic hyperplasia[97] and the pain associated with osteoarthritis.[98] In-vitro tests show antiinflammatory action.[99] In a rodent model, stinging nettle reduced LDL cholesterol and total cholesterol. [100] In another rodent study it reduced platelet aggregation.[101]
- Valerian root can be used to treat insomnia. Clinical studies show mixed results and researchers note that many trials are of poor quality.[102][103][104]
- Vanilla
- Ocimum gratissimum[105][106] and tea tree oil can be used to treat acne.
- Green tea components may inhibit growth of breast cancer cells[107] and may heal scars faster.[108]
- Lemon grass can lower cholesterol.[citation needed]
- Honey may reduce cholesterol.[109] May be useful in wound healing.[110]
Risks
Proper double-blind clinical trials are needed to determine the safety and efficacy of each plant before they can be recommended for medical use.[111] In addition, many consumers believe that herbal medicines are safe because they are natural. Herbal medicines may interact with synthetic drugs causing toxicity to the patient, herbal products may have contamination that is a safety consideration, and herbal medicines, without proven efficacy, may be used to replace medicines that have a proven efficacy.[48]
Standardization of purity and dosage is not mandated in the United States, but even products made to the same specification may differ as a result of biochemical variations within a species of plant.[112] Plants have chemical defense mechanisms against predators that can have adverse or lethal effects on humans. Examples of highly toxic herbs include poison hemlock and nightshade.[113] They are not marketed to the public as herbs, because the risks are well known, partly due to a long and colorful history in Europe, associated with "sorcery", "magic" and intrigue.[114] Although not frequent, adverse reactions have been reported for herbs in widespread use.[115] On occasion serious untoward outcomes have been linked to herb consumption. A case of major potassium depletion has been attributed to chronic licorice ingestion.[116] Black cohosh has been implicated in a case of liver failure.[117]Few studies are available on the safety of herbs for pregnant women.[118][119]
Herb drug interactions are a concern. In consultation with a physician, usage of herbal remedies should be clarified, as some herbal remedies have the potential to cause adverse drug interactions when used in combination with various prescription and over-the-counter pharmaceuticals.
Dangerously low blood pressure may result from the combination of an herbal remedy that lowers blood pressure together with prescription medicine that has the same effect. Some herbs may amplify the effects of anticoagulants.[120] Certain herbs as well as common fruit interfere with cytochrome P450, an enzyme critical to drug metabolism.[121]
Effectiveness
The gold standard for pharmaceutical testing is repeated, large-scale, randomized, double-blind tests. Some plant products or pharmaceutical drugs derived from them are incorporated into mainstream medicine. To recoup the considerable costs of testing to the regulatory standards, the substances are patented by pharmaceutical companies and sold at a substantial profit.[122]
Most herbal traditions have developed without modern scientific controls to distinguish between the placebo effect, the body's natural ability to heal itself, and the actual benefits of the herbs themselves.[citation needed] Many herbs have shown positive results in in-vitro, animal model or small-scale clinical tests[123] but many studies on herbal treatments have also found negative results.[124] The quality of the trials on herbal remedies is highly and many trials of herbal treatments have been found to be of poor quality, with many trials lacking a intention to treat analysis or a comment on whether blinding was successful.[125] The few randomized, double-blind tests that receive attention in mainstream medical publications are often questioned on methodological grounds or interpretation. Likewise, studies published in peer-reviewed medical journals such as Journal of the American Medical Association receive more consideration than those published in specialized herbal journals. This preference may be due to the possibility of location bias for such trials. One study found that non-impact factor alternative medicine journals published more studies with positive results than negative results and that trials finding positive results were of lower quality than trials finding negative results. High impact factor mainstream medical journals, on the other hand, published equal numbers of trials with positive and negative results. In high impact journals, trials finding positive results were also found to have lower quality scores than trials finding negative results.[126] Another study found studies of phyomedicine to have superior quality to matched studies of pharmaceuticals.[127] However, this study used a matched pair design and excluded all herbal trials that were not controlled, did not use a placebo or did not use random or quasi random assignment.
Herbalists criticize mainstream studies on the grounds that they make insufficient use of historical use. They maintain that tradition can guide the selection of factors such as optimal dose, species, time of harvesting and target population.[128]
Dosage is in general an outstanding issue for herbal treatments: while most conventional medicines are heavily tested to determine the most effective and safest dosages (especially in relation to things like body weight, drug interactions, etc.), there are few established dosage standards for various herbal treatments on the market.[citation needed] Furthermore, herbal medicines taken in whole form cannot generally guarantee a consistent dosage or drug quality (since certain samples may contain more or less of a given active ingredient.
Several methods of standardization may be applied to herbs. One is the ratio of raw materials to solvent. However different specimens of even the same plant species may vary in chemical content. Another method is standardization on a signal chemical.[129]
Clinical studies
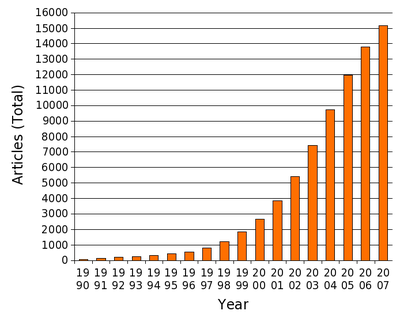
In 2004 the U.S. National Center for Complementary and Alternative Medicine of the National Institutes of Health began funding clinical trials into the effectiveness of herbal medicine.[130]
Name confusion
context would be used for weight loss or given for long periods of time.
In Chinese medicine these herbs are used for certain forms of acute arthritis and edema.[133][134][135]
Standards and quality control
The issue of regulation is an area of continuing controversy in the EU and USA. At one end of the spectrum, some herbalists maintain that traditional remedies have a long history of use, and do not require the level of safety testing as xenobiotics or single ingredients in an artificially concentrated form.[citation needed] On the other hand, others are in favor of legally enforced quality standards, safety testing and prescription by a qualified practitioner.[citation needed] Some professional herbalist organizations have made statements calling for a category of regulation for herbal products.[136] Yet others agree with the need for more quality testing but believe it can be managed through reputation without government intervention.[137]The legal status of herbal ingredients varies by country.
In the United States, most herbal remedies are regulated as dietary supplements by the Food and Drug Administration.[citation needed] Manufacturers of products falling into this category are not required to prove the safety or efficacy of their product, though the FDA may withdraw a product from sale should it prove harmful.[138][139]
The National Nutritional Foods Association, the industry's largest trade association, has run a program since 2002, examining the products and factory conditions of member companies, giving them the right to display the GMP (Good Manufacturing Practices) seal of approval on their products.[140]
In the UK, herbal remedies that are bought over the counter are regulated as supplements, as in the US[citation needed]. However, herbal remedies prescribed and dispensed by a qualified "Medical Herbalist", after a personal consultation, are regulated as medicines.
A Medical Herbalist can prescribe some herbs which are not available over the counter, covered by Schedule III of the Medicines Act[citation needed]. Forthcoming changes to laws regulating herbal products in the UK, are intended to ensure the quality of herbal products used[citation needed].
Some herbs, such as cannabis, however, are outright banned in most countries for various reasons. Since 2004, the sales of ephedra as an herbal supplement is prohibited in the United States by the FDA.[141]
Danger of extinction
On January 18, 2008, the Botanic Gardens Conservation International (representing botanic gardens in 120 countries) stated that "400 medicinal plants are at risk of extinction, from over-collection and deforestation, threatening the discovery of future cures for disease." These included Yew trees (the bark is used for cancer drugs, paclitaxel); Hoodia (from Namibia, source of weight loss drugs); half of Magnolias (used as Chinese medicine for 5,000 years to fight cancer, dementia and heart disease); and Autumn crocus (for gout). The group also found that 5 billion people benefit from traditional plant-based medicine for health care[142]
See also
- Anesthesia
- Ayurveda
- Chinese herbology
- Doctrine of signatures
- Ethnobotany
- Gemmotherapy
- History of alternative medicine
- Home remedy
- Homeopathy
- King's American Dispensatory
- List of plants used as medicine
- Naturopathic medicine
- Pharmacognosy


















No comments:
Post a Comment